Brief Mindfulness-based Interventions for Acute and Chronic Pain a Systematic Review
Effectiveness of Mindfulness-Based Interventions on Pain Intensity in Patients with Chronic Low Back Pain: A Systematic Review
Abstract
Context:
Chronic depression back hurting (CLBP) is the most prominent cause of disability worldwide. For the treatment of CLBP, Mindfulness-based Interventions (MBIs) such as mindfulness-based stress reduction (MBSR), mindfulness-based cognitive therapy (MBCT), mindfulness meditation (MM) are often used; still, their verbal effect on pain intensity has not yet been determined for these people.
Objectives:
This study aimed to evaluate the effectiveness of MBIs on pain intensity in people with CLBP.
Data Sources:
In this systematic review, all of the randomized controlled trials available on PubMed, PsycInfo, Cochrane Library, Google Scholar, Scopus, and ProQuest databases from 2014 to 2020 were reviewed. This study is too the showtime review article in the field of chronic depression back pain that reviews the databases of Google Scholar, Irandoc, and SID in Farsi.
Study Selection:
Studies were included if they were: (1) RCT; (ii) had patients with chronic low back hurting; (3) made a comparison between MBIs and a passive comparator (usual intendance) or an active comparator (such as cerebral-behavioral therapy (CBT) or health pedagogy); (4) examined pain intensity.
Results:
In the initial search, we found 297 trials in total databases. After removing duplicates and applying all inclusion and exclusion criteria, 9 RCT (totaling 959 patients) with CLBP were included for this systematic review.
Conclusions:
MBIs are effective solutions for coping with CLBP, and their furnishings are maintained for a long fourth dimension. No significant divergence was found betwixt the effectiveness of these treatments and CBT treatment on hurting intensity of patients with CLBP.
Keywords
Chronic Depression Back Pain Interventions Mindfulness-Based Interventions
1. Context
Low back pain (LBP) is one of the about usual causes for which people follow medical treatments. It is estimated that i in two people volition experience LBP throughout their lifetime, and at least 10% of LBP sufferers feel chronic low back pain (CLBP) (ane). In 2015, the worldwide prevalence of disability due to LBP was 7.3%, which means that 540 million people are affected past LBP. In fact, LBP is the most prominent cause of disability worldwide (2). The majority of LBP sufferers are between 40 and 80 years old (3). Moreover, CLBP is associated with disability, depression, cognitive dysfunctional, loss of sleep and appetite, and social isolation (4). In improver to human suffering, high economical costs of wellness-care and indirect costs of job loss or productivity decrease can be counted every bit other crises of chronic pain (5-nine).
In the treatment of CLBP, ordinary treatments such every bit pharmacological, medical, surgical, are not solely effectual in the emptying of pain or improving emotional and physical functioning (x). International guidelines about CLBP care have focused on treatments that emphasize the active function of patients, including practise, relaxation, and behavioral changes due to psychological treatments (11). Among psychological treatments, CBT has more bear witness in chronic hurting research literature. As chronic pain has a complex nature, CBT, like medical treatments, cannot be influential in eliminating and controlling pain (12).
Unlike other treatments, which focus on diminishing and controlling the intensity of the pain, mindfulness-based interventions (MBIs) helps patients without requiring to modify pain intensity (13). MBIs taken from ancient Buddha have attracted much attention in contemporary psychotherapy. Mindfulness with the attitude of not-judgmental acceptance is a miracle that requires one'south full consciousness. That awareness is accompanied by a careful observation of perceptions, cognitions, emotions, or feelings without skilful or bad evaluation, correct or wrong, salubrious or ill, important, or unimportant (14). Two concepts have been identified in mindfulness: cocky-regulation of attention and orientating to the present moment with curiosity, openness, and credence (15). Humans normally are not aware of their moment-by-moment experiences; they seem to be in an automobile-pilot manner. Moment-past-moment awareness of experiences can enrich the sense of life in which each experience tin be an alive and active mental partnership rather than a subconscious response (16).
The question is whether MBIs with a focus on improving function and active role of the patient can reduce the pain intensity in patients with CLBP. The effectiveness of MBIs in hurting intensity in patients with chronic pain is investigated in a review article by Reiner et al. (13). This study reviews 16 articles, 10 of which showed a meaningful reduction in pain intensity of the MBIs groups.
2. Objectives
In this systematic review, we aimed to investigate whether MBIs have been able to reduce short term and long term pain intensity in people with CLBP. Too, since there is not whatever review article which investigates Persian articles on this topic, we will too have a Farsi search which can heighten the quality of this review.
3. Data Sources
3.1. Search Strategy
We searched six databases, including MEDLINE/PubMed, Cochrane Library, PsycINFO, GoogleScholar, Scopus, and ProQuest in English and Irandoc, Google Scholar, and SID databases in Persian from 2014 to June 2020. The following terms were searched in English databases: MBSR [Title/Abstruse] OR MBCT [Championship/Abstract] OR Mindfulness [Title/Abstract] OR Meditation [Title/Abstract] AND Low Dorsum Pain [Championship/Abstract] OR Lower Back Hurting [Title/Abstract] OR Lumbago [Title/Abstruse] OR Low Backache [Championship/Abstract] OR Low Back Anguish [Championship/Abstract] OR Mechanical Depression Dorsum Pain [Title/Abstract] OR Postural Low Back Pain [Title/Abstruse] OR Recurrent Low Back Pain [Title/Abstract]. Nosotros also searched the following terms in Persian databases: Mindfulness [Title/Abstract] OR MBSR [Title/Abstract] OR MBCT [Title/Abstract] AND chronic low dorsum pain [Title/Abstract]. The reference lists of identified original articles or reviews were also examined manually for boosted eligible studies.
four. Study Pick
Studies were included if they were: (1) RCT; (2) had patients with CLBP of whatsoever reason, duration, or intensity; (3) made a comparing between MBIs and a passive comparator (usual care) or an active comparator (such equally cognitive-behavioral therapy (CBT) or wellness didactics); (four) examined pain intensity.
Studies were excluded if they were: (ane) non-randomized trials or observational studies; (2) interventions included individual therapy sessions; (three) had not been published as a total-text; (four) used interventions that had no formal meditation (for instance, acceptance and commitment therapy or dialectic behavioral therapy); (5) interventions included other meditations such as yoga, tai chi, qigong, or meditation techniques without referring to the mindfulness. Two reviewers (F.A. and Chiliad.H.) independently reviewed all of the recovered articles in full to determine their eligibility for inclusion. Discrepancies between the reviewers were resolved past consensus of the third reviewer (H.H.).
five. Data Extraction
Two reviewers independently extracted information from the eligible articles. We studied total texts of the concluding manufactures and extracted some information about commodity characteristics (including trial design and randomization), sample characteristics (including sample size, age, sex activity, and diagnosis), intervention and comparison group characteristics (including type, program length, and frequency and duration of sessions), pain intensity characteristics (type of measuring tool, short and long-term outcomes), and information about follow-upward length and outcome. Discrepancies between the reviewers were resolved by consensus of the third reviewer (H.H.).
5.1. Assessment of the Risk of Bias
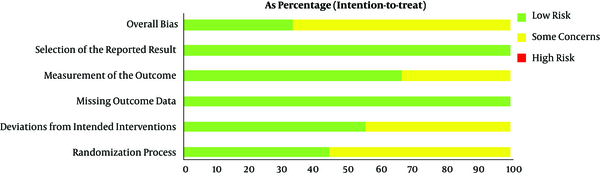
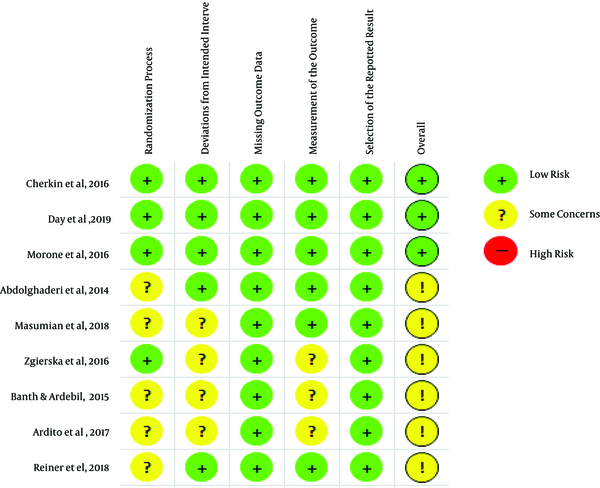
Two reviewers independently evaluated the take chances of bias based on the Cochrane risk-of-bias tool for randomized trials (RoB 2) in terms of the randomization process, deviations from the intended interventions, missing upshot data, measurement of the effect, and choice of the reported result. Discrepancies between the reviewers were resolved by consensus of the third reviewer (H.H.).
6. Results
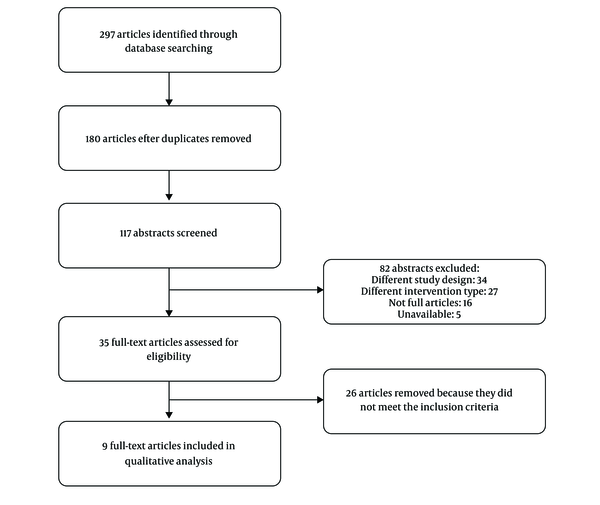
A total of 297 relevant articles were retrieved by the initial search, among which 262 duplicate and irrelevant manufactures were deleted afterward reviewing their titles and abstracts. After full-text evaluation, 26 studies were excluded due to the lack of inclusion criteria mentioned in the methodology. Eventually, 9 articles with a total of 959 patients were included in this systematic review (Effigy 1).
The characteristics of the nine studies are shown in Tables 1 and 2. In this written report, patients with CLBP ranged between 20 and seventy years of age, but ane RCT enrolled patients older than 65 years (17), and another enrolled twenty - 80 years old (18). In RCTs, the duration of pain was reported from three months or more (17-22), six months or more (23), and in ii RCT is non mentioned (24, 25). They were referred either through physicians in rehabilitation centers, adult hurting clinics, and physiotherapy centers (xviii, 20, 21, 23, 25), or they have introduced themselves afterward having been informed through a variety of media such as paper ads, directly postal service (such as letters, brochures, Emails), or phone calls (17, 19, 20, 22).
| Authors/Yr | Participants (Groups) | Mean (SD) Age, y | Inclusion Criteria | Mindfulness Intervention | Treatment Grouping (Intervention Length, Frequency, Duration) |
|---|---|---|---|---|---|
| Banth and Ardebil, 2015 (23) | 88 (2) | Overall: 40.iii (eight.2) | Historic period xxx - 45 years, being under medical treatments, history of non-specific low dorsum pain persisting pain for ≥ half-dozen months, language-Farsi, gender-female, educated at to the lowest degree upward to high school. | MBSR | MBSR, an viii-week program, 1 session per week for 90min; Homework: 30 - 45 min daily |
| Cherkin et al., 2016 (xix) | 342 (3) | UC: 48.9 (12.5); MBSR: 50.0 (11.9); CBT: 49.1 (12.6) | twenty to lxx years of age, with non-specific depression dorsum hurting that persisted for ≥ three months, rated pain bothersomeness ≥ 4 on 0- to 10-signal scales, pain interference with activities ≥ 3 on 0- to 10-betoken scales | MBSR | MBSR, an 8-week program, once weekly for 2 hours plus optional 6 hours retreat. homework: frequency and duration not mentioned |
| Zgierska et al., 2016 (22) | 35 (ii) | Overall: 51.8 (ix.vii) | Historic period ≥ 21 years, fluent in English language, daily CLBP for ≥ 3 months, daily opioid therapy (at to the lowest degree 30 mg/twenty-four hour period of MED), and ability to feel thermal sensations in both hands | Mindfulness meditation-CBT intervention | Meditation-CBT intervention, 2 hours per week for 8 weeks; homework: at least half dozen days per week for at least 30 minutes per 24-hour interval |
| Morone et al., 2016 (17) | 282 (2) | MBSR: 75 (vii.2); GC: 74 (6.0) | Historic period ≥ 65 years, spoke English, Mini-Mental Country Examination score ≥ 24, RMDQ ≥ xi, CLBP (with moderate intensity for ≥ 3 months, occurring daily or most every day) | MBSR | MBSR, an eight-calendar week program, one session per calendar week for 90 min, subsequently intervention monthly 60-minute booster sessions, homework: daily meditation (six of seven days/calendar week) lasting 50 minutes (45 minutes of meditation, 5 minutes to complete a log) |
| Ardito et al., 2017 (21) | 28 (2) | Overall: 48.14 (11.09) | twenty to 65 years of age, CLBP for ≥ 3 months, etiology of the hurting: lumbago, sciatica due to deportation of the intervertebral disc, neuralgia, neuritis, radiculitis due to displacement or rupture of the lumbar intervertebral disc, lumbosacral spondylosis without myelopathy or fibromyalgia | MBSR | MBSR, viii weekly sessions of two hours and during the second-to-last weekend a 7-60 minutes session; homework: 40 min a twenty-four hour period |
| Masumian et al., 2018 (24) | 18 (2) | MBSR: 44.33 (10.22); CG: 51 (3.42) | 18 to 60 years of age | MBSR | MBSR, one solar day a week during 2 - 2.5 hours in 8 sessions; homework: frequency and duration not mentioned |
| Mean solar day et al., 2019 (twenty) | 69 (3) | MM: 48.09 (16.13); MBCT: 49.87 (11.89); CT: 54.26 (14.87) | Age ≥ 18 years, a primary trouble of CLBP (hurting lasting for ≥ 3 months, experienced on ≥ 50% of days), average pain intensity of ≥ four for most days of the previous three months, analgesic or psychotropic medications have been stabilized for four or more weeks before study enrollment, fluent in English language, able to attend a weekly two-hour therapy. | MM, MBCT | MM, MBCT intervention, 8 weekly two-hour sessions, Homework: 45 minutes, six days per week. |
| Abdolghadery et al., 2014 (25) | thirty (3) | CLBP was diagnosed past a specialist doctor, ages 18 to 60 years, upper secondary education, and No substance abuse. | MBCT | MBCT, each week for a ninety-minute session for viii weeks; homework: frequency and duration not mentioned | |
| Reiner et al., 2018 (eighteen) | 67 (ii) | CLBP for ≥ three months, pain level score of ≥ v | MBI | Inspired by MBSR and MBCT, each calendar week for a ninety-minute session for eight weeks; homework: practice daily for at to the lowest degree twenty min |
Abbreviations: CBT, cognitive behavioral therapy; MBSR, mindfulness-based stress reduction; MM, mindfulness meditation; SD, standard divergence.
| Comparing Group (Intervention Length, Frequency, Duration) | Longest Follow-Up | Pain Intensity Measures | Results on Pain Intensity |
|---|---|---|---|
| Usual intendance only | 1 month | McGill Pain questionnaire | Significant differences for MBSR vs. UC in short- and long-term |
| ane) CBT techniques near commonly applied and studied for chronic low back pain, an 8-calendar week program, once weekly for two hours. Homework: Frequency and duration not mentioned; 2) Usual care only | 26 and 52 weeks | Average of iii ratings (current, worst, and average back pain in the previous month) rated on an 11-point Numerical Rating calibration. | Pregnant differences; for MBSR vs. UC in; short- and long-term, no significant; differences for MBSR; vs. CBT |
| Usual care only | 26 weeks | Average of four-detail subscale from the Brief Hurting Inventory: "current" and by-week "average, worst and least" pain intensity, rated on an 11-signal Numerical Rating scale. | Meaning differences for meditation-CBT intervention vs. UC in short- and long-term (P = 0.045) |
| Viii weekly 90-minute wellness education program based on the "10 keys" to healthy crumbling, after intervention monthly 60-minute booster sessions; homework: frequency and elapsing not mentioned | Six months | present, average, and most astringent during the past week by self-written report with the Numeric Hurting Rating calibration (NRS; range, 0 - 20) | Significant differences for MBSR vs. health pedagogy programme in long-term electric current and well-nigh severe pain intensity in the past week. |
| Usual intendance only | iv - v months | The Numeric Rating scale (NRS), scale from 0 ("no hurting at all") to 100 ("my pain is equally bad equally it could peradventure be"). | Significant differences were observed for MBSR vs. UC in brusque- and long-term |
| Usual intendance but | 0 | Multidimensional pain inventory (MPI) | Significant differences for MBSR vs. UC in terms of these subscales (daily action disorder, pain intensity, and control over life) [P < 0.05], but not whatever difference between groups in terms of social support and emotional distress subscales [P > 0.05] |
| 1) Eight weekly 2 hours CT sessions homework: 45-minute, half-dozen days per calendar week. two) 8 weekly ii hours of MM sessions; Homework: 45 minutes, six days per week. | Iii months and 6 months | Average of four pain intensity items: about astringent pain, to the lowest degree severe pain, average pain over the past week, and electric current pain rated on an 11-betoken Numerical Rating Calibration. | Significant differences for post- vs. pre-treatment in MBCT, MM, CT groups in short- and long-term, with no significant differences between groups. |
| 1) Viii weekly xc minutes CBT sessions; 2) usual care | 0 | McGill Pain questionnaire | Meaning differences; for MBCT vs. UC in; short-term, No meaning; differences for MBSR; vs. CBT. |
| Usual care merely | Three months | Brief pain inventory, thermal sensory analyzer, warm awareness threshold and heat pain threshold, supra threshold pain | According to brief pain inventory, significant differences were observed for MBI vs. UC. |
In intervention groups, the type of MBIs is not the aforementioned in different studies; amid them, mindfulness-based stress reduction (MBSR) (17, 19, 21, 23, 24), combined Mindfulness-Based Stress Reduction and CBT (MBSR/CBT) (22), Mindfulness-Based cognitive Therapy (MBCT) (20, 25), Mindfulness Meditation (20), and combined MBIs (MBSR/MBCT) (eighteen) were used in intervention groups. MBIs were conducted in eight weeks and consisted of one two-2.v-hour session per calendar week, except for four RCTs, which held MBIs at one 90-infinitesimal session per week (17, 18, 23, 25). Almost one-half of each session was devoted to mindfulness meditation (torso scanning, sitting meditation, and walking meditation) and the other one-half to training and conversation. All studies in their intervention groups required homework. In almost of the studies, homework involved 30 - 45 minutes of meditation for 6 days a calendar week (17, 20-23), except for one RCT, which involved twenty minutes of meditation for practice daily (18). In the rest of the studies, its period and frequency were not mentioned.
Different pain measurement tools take been used in different studies: McGill Pain questionnaire (23, 25), Numeric Rating scale (NRS) (17, nineteen-21), brief pain inventory (xviii, 22), and multidimensional pain inventory (MPI) (24).
In the first trial, 342 patients with CLBP in MBSR, CBT, and usual care groups were compared. Patients in the MBSR grouping showed a significant comeback in low back pain at 26 weeks compared to the usual care group (hateful departure (Doc), -0.64 [confidence interval (CI), -1.18 to -0.11]) and this improvement was maintained at 52 weeks (MD, -0.85 [CI, -1.39 to -0.32]). In this trial, no notable differences were observed between MBSR and CBT (19). The second trial compared the effects of mindfulness meditation (MM), cognitive therapy (CT), and mindfulness-based cerebral therapy (MBCT) treatments on 69 patients who had been suffering from CLBP for an average of 14 years. Comparison postal service-treatment and pre-handling for n = 43 (follow-up samples), meaningful improvements in pain intensity were illustrated in MBCT group (0.88 MD, [CI, 0.19 to 1.58]) and in MM group (Medico, 0.41 [CI, -0.36 to 1.eighteen]). This improvement was maintained at 3-month (MBCT (MD, 1.14 [CI, 0.38 to one.89]), MM (MD, 0.48 [CI, -0.36 to 1.31])) and 6-month follow-up (MBCT (MD, 1.37 [CI, 0.67 to 2.07]), MM (MD, 0.81 [CI, 0.04 to 1.59])). No significant differences were found betwixt the three handling groups (20). In the third trial, the efficacy of MBSR was compared with the Health Education program in 282 patients with CLBP over the age of 65 years. The MBSR group showed a significant reduction in electric current and most astringent pain for the past week during the 6-month follow-upwardly. The changes in mean pain intensity were not significant (-0.ane [95% CI, -1.i to i.0] at 8 weeks and -i.1 [95% CI, -2.two to -0.01] at 6 months) (17). In another trial with a small group of 28 patients with CLBP, the efficacy of MBSR on pain intensity, endocrine, and mental and physical functions were compared with the control group. The study showed moderate to high improvements in four - five months of follow-up in pain intensity and physical and psychological functioning (21). In a trial among patients with CLBP (northward = 35) undergoing opioid treatment (at least xxx mg/day), the efficacy of CBT-mindfulness meditation intervention was compared with usual care. Afterward 8 weeks of intervention (MD, 0.ix [CI 0.01 to 1.vii] and 26 weeks (Dr., 1.03 [CI 0.2 to i.9]), meaning differences in hurting intensity between the command grouping and the experimental group were observed (22). In this trial, patients were categorized equally either "consistent" meditators ( ≥ 150 minutes/calendar week of formal meditation practice during at least ii/3 of the study) or "inconsistent" meditators (< 150 minutes/week of practice during at least 2/3 of the study). Compared to the command group, the consistent group showed a significant reduction in pain intensity at 26 weeks of follow-up, and the inconsistent group showed transient comeback at 8 weeks; but, these 2 groups (both in self-reported and in Biomarker measurements) were not significantly dissimilar between the consistent and inconsistent meditators at 8 and 26 weeks.
Some other study compared 30 patients with CLBP in CBT, MBCT, and usual intendance groups. Sensory, emotional, and neuropathic pain intensity in CBT and MBSR groups showed a significant improvement compared to the command group, but no meaning difference was found between CBT and MBCT (25). A modest group of 18 patients with CLBP was compared in two groups of MBSR and usual care. In this trial, Multidimensional Pain Inventory (MPI) questionnaire was used to assess their pain intensity, which showed that MBSR improved pain intensity, daily activeness disorder, and control over life subscales compared to usual care, merely there was no significant deviation in social support and emotional distress subscales (24). Finally, in a study, quantitative sensory pain testing (QST) measures of the thermal and pain thresholds, pain ratings to fixed stimuli, self-report measures of the chronic pain severity, and interference with daily activities were adamant at baseline after viii weeks. The MBI group indicated a subtract in ratings, while the command group indicated an increment (xviii). The overall take chances of bias was "low" in three studies (17, 19, xx) and "some concerns" in other studies (Figures 2 and 3).
7. Discussion
This current systematic review is the simply report that investigates the effectiveness of MBIs on CLBP in both English and Farsi languages. The results showed that among patients with CLBP, MBIs compared to usual care significantly reduced pain intensity both statistically and clinically. Assessments also showed that MBIs reduced pain intensity as efficiently equally CBT and there was no statistically significant deviation between them. These results are consistent with the findings of a systematic review by Rainer et al., which reviewing controlled and uncontrolled trials, the issue of MBIs on pain intensity in patients with chronic pain is demonstrated (13).
Mind-torso treatments such as MBSR and CBT are aimed at managing pain and equipping patients with effective long-term skills (19). By reviewing follow-up periods, we concluded that the efficacy of MBIs in reducing pain intensity was besides maintained in a long period. A meta-analysis and systematic review showed in the curt term, MBSR finer reduces the pain intensity in patients with CLBP just failed to maintain this efficacy in the long term (26). The result shown in this written report is different from the evidence in our study, which may exist due to the pocket-size number of articles reviewed by this review study.
In most of the studies reviewed in this review article, hurting intensity has been investigated as the primary effect. It should be noted that reduction in hurting intensity is not the primary focus of MBIs; in fact, these interventions reduce hurting intensity indirectly by teaching patients to alter their perspective about hurting (27). Too, it was shown (28) that the reduction in pain intensity associated with meditation is directly related to the part of the encephalon where the pain is diagnosed. This commodity states that mindfulness skills change the mental feel of pain.
Of the viii studies reviewed, simply one study examined the effectiveness of mindfulness in people over 65 years of historic period (17). The results showed that MBSR did not significantly affect average pain intensity. A systematic and meta-analysis review, investigating the effectiveness of various interventions on elderly people with non-specific CLBP, showed that complementary health approach (such every bit acupuncture, mindfulness, yoga, etc.) was not effective for pain intensity and disability in the elderly (29). Among the articles reviewed in this review written report, there is but one article that uses mindfulness to treat elderly people with non-specific CLBP, then it tin can be said that evidence is express to appraise the effectiveness of mindfulness on older adults, and it needs farther investigation.
In search of the Western farsi language, but 1 related commodity was extracted between the mentioned years in which the sample size was small and did non have a follow-up menstruation. Therefore, it is recommended that more than studies with larger sample sizes and longer duration of follow-up should be performed for evaluation of the effectiveness of MBI on the pain intensity in chronic depression back pain.
8. Limitations
The limitations of the reviewed articles are the depression sample size, college education level, short follow-up courses, or sometimes no follow-up courses. The limitations of the present report are the heterogeneity of age and gender of participants, the tools of measuring pain intensity, and the blazon of intervention in the comparative group.
9. Conclusions
The results evidence that among patients with CLBP, MBI reduces pain intensity in short and long periods. It is too shown that the effectiveness of MBIs for pain intensity in CLBP is similar to CBT and is non significantly different.
References
- ane.
Vitoula M, Venneri A, Varrassi G, Paladini A, Sykioti P, Adewusi J, et al. Behavioral Therapy Approaches for the Direction of Low Dorsum Pain: An Up-To-Date Systematic Review. Pain Ther. 2018;7(1):ane-12. doi: 10.1007/s40122-018-0099-four. [PubMed: 29767395]. [PubMed Central: PMC5993685].
- 2.
Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, et al. What depression back pain is and why we need to pay attention. Lancet. 2018;391(10137):2356-67. doi: 10.1016/s0140-6736(xviii)30480-ten.
- 3.
Hoy D, Bain C, Williams Thousand, March L, Brooks P, Blyth F, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012;64(6):2028-37. doi: 10.1002/art.34347. [PubMed: 22231424].
- 4.
Luiggi-Hernandez JG, Woo J, Hamm M, Greco CM, Weiner DK, Morone NE. Mindfulness for Chronic Low Back Pain: A Qualitative Analysis. Pain Med. 2018;19(xi):2138-45. doi: 10.1093/pm/pnx197. [PubMed: 29025059]. [PubMed Fundamental: PMC6659019].
- 5.
Van Den Kerkhof EG, Hopman WM, Towheed TE, Anastassiades TP, Goldstein DH, Canadian Multicentre Osteoporosis Study Enquiry G. The impact of sampling and measurement on the prevalence of cocky-reported hurting in Canada. Pain Res Manag. 2003;8(3):157-63. doi: 10.1155/2003/493047. [PubMed: 14657983].
- 6.
Colombo GL, Caruggi Yard, Vinci M. [Quality of life and treatment costs in patients with non-cancer chronic hurting]. Recenti Prog Med. 2004;95(11):512-20. Italian.
- vii.
Corcoll J, Orfila J, Tobajas P, Alegre L. Implementation of neuroreflexotherapy for subacute and chronic neck and back pain within the Spanish public health organization: inspect results after 1 yr. Health Policy. 2006;79(2-3):345-57. doi: 10.1016/j.healthpol.2005.11.001. [PubMed: 16563551].
- 8.
Shipton EA, Tait B. Flagging the pain: preventing the burden of chronic pain past identifying and treating adventure factors in acute pain. Eur J Anaesthesiol. 2005;22(6):405-12. doi: x.1017/s0265021505000694. [PubMed: 15991501].
- 9.
Qaseem A, Wilt TJ, McLean RM, Forciea MA, Clinical Guidelines Committee of the American College of P. Noninvasive Treatments for Astute, Subacute, and Chronic Low Back Hurting: A Clinical Exercise Guideline From the American Higher of Physicians. Ann Intern Med. 2017;166(7):514-xxx. doi: 10.7326/M16-2367. [PubMed: 28192789].
- 10.
Turk DC, Wilson HD, Cahana A. Handling of chronic non-cancer pain. Lancet. 2011;377(9784):2226-35. doi: x.1016/s0140-6736(11)60402-ix.
- 11.
Clement I, Lorenz A, Ulm B, Plidschun A, Huber South. Implementing Systematically Collected User Feedback to Increment User Retentivity in a Mobile App for Self-Management of Low Back Pain: Retrospective Accomplice Study. JMIR Mhealth Uhealth. 2018;6(6). e10422. doi: 10.2196/10422. [PubMed: 29875088]. [PubMed Central: PMC6010841].
- 12.
Veehof MM, Trompetter Hr, Bohlmeijer ET, Schreurs KM. Acceptance- and mindfulness-based interventions for the treatment of chronic pain: a meta-analytic review. Cogn Behav Ther. 2016;45(1):5-31. doi: x.1080/16506073.2015.1098724. [PubMed: 26818413].
- xiii.
Reiner K, Tibi L, Lipsitz JD. Do mindfulness-based interventions reduce pain intensity? A critical review of the literature. Pain Med. 2013;14(ii):230-42. doi: 10.1111/pme.12006. [PubMed: 23240921].
- 14.
Baer RA. Mindfulness Training as a Clinical Intervention: A Conceptual and Empirical Review. Clin Psychol-Sci Pr. 2006;ten(2):125-43. doi: 10.1093/clipsy.bpg015.
- 15.
Bishop SR, Lau K, Shapiro South, Carlson L, Anderson ND, Carmody J, et al. Mindfulness: A proposed operational definition. Clin Psychol-Sci Pr. 2006;eleven(3):230-41. doi: ten.1093/clipsy.bph077.
- 16.
Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits. J Psychosom Res. 2004;57(ane):35-43. doi: x.1016/s0022-3999(03)00573-7.
- 17.
Morone NE, Greco CM, Moore CG, Rollman BL, Lane B, Morrow LA, et al. A Heed-Body Plan for Older Adults With Chronic Low Dorsum Pain: A Randomized Clinical Trial. JAMA Intern Med. 2016;176(three):329-37. doi: 10.1001/jamainternmed.2015.8033. [PubMed: 26903081]. [PubMed Fundamental: PMC6361386].
- 18.
Reiner K, Shvartzman P, Cohen ZZ, Lipsitz JD. Assessing the Effectiveness of Mindfulness in the Handling of Chronic Dorsum Hurting: Use of Quantitative Sensory Hurting Assessment. Mindfulness. 2018;10(5):943-52. doi: 10.1007/s12671-018-1053-6.
- 19.
Cherkin DC, Sherman KJ, Balderson BH, Cook AJ, Anderson ML, Hawkes RJ, et al. Effect of Mindfulness-Based Stress Reduction vs Cognitive Behavioral Therapy or Usual Care on Back Pain and Functional Limitations in Adults With Chronic Low Back Hurting: A Randomized Clinical Trial. JAMA. 2016;315(12):1240-nine. doi: x.1001/jama.2016.2323. [PubMed: 27002445]. [PubMed Fundamental: PMC4914381].
- twenty.
Day MA, Ward LC, Ehde DM, Thorn BE, Burns J, Barnier A, et al. A Pilot Randomized Controlled Trial Comparing Mindfulness Meditation, Cognitive Therapy, and Mindfulness-Based Cognitive Therapy for Chronic Low Back Pain. Pain Med. 2019;20(11):2134-48. doi: ten.1093/pm/pny273. [PubMed: 30605517].
- 21.
Ardito RB, Pirro PS, Re TS, Bonapace I, Menardo V, Bruno Due east, et al. Mindfulness-Based Stress Reduction Plan on Chronic Low-Dorsum Pain: A Study Investigating the Impact on Endocrine, Physical, and Psychologic Functioning. J Altern Complement Med. 2017;23(8):615-23. doi: ten.1089/acm.2016.0423. [PubMed: 28537422].
- 22.
Zgierska AE, Burzinski CA, Cox J, Kloke J, Stegner A, Cook DB, et al. Mindfulness Meditation and Cerebral Behavioral Therapy Intervention Reduces Hurting Severity and Sensitivity in Opioid-Treated Chronic Low Back Pain: Pilot Findings from a Randomized Controlled Trial. Pain Med. 2016;17(10):1865-81. doi: x.1093/pm/pnw006. [PubMed: 26968850]. [PubMed Central: PMC5063022].
- 23.
Banth S, Ardebil Physician. Effectiveness of mindfulness meditation on pain and quality of life of patients with chronic depression back hurting. Int J Yoga. 2015;eight(2):128-33. doi: 10.4103/0973-6131.158476. [PubMed: 26170592]. [PubMed Key: PMC4479890].
- 24.
Masumian S, Shairi M, Ghahari South, Rajabi M, Mazloumi F. [The effects of mindfulness-based stress reduction therapy on chronic low back hurting patients]. An -Noor London. 2018;22(two):105-eleven. Persian.
- 25.
Abdolghadery 1000, Kafee M, Saberi A, Aryapouran S. [The effectiveness of mindfulness-based cognitive therapy (mbct) and cerebral behavior therapy (CBT) on decreasing pain, depression and anxiety of patients with chronic low back pain]. J Shahid Sadoughi Univ Med Sci. 2014;21(half dozen):795-807. Persian.
- 26.
Anheyer D, Haller H, Barth J, Lauche R, Dobos Chiliad, Cramer H. Mindfulness-Based Stress Reduction for Treating Low Back Pain: A Systematic Review and Meta-analysis. Ann Intern Med. 2017;166(11):799-807. doi: 10.7326/M16-1997. [PubMed: 28437793].
- 27.
Veehof MM, Oskam MJ, Schreurs KM, Bohlmeijer ET. Acceptance-based interventions for the handling of chronic pain: a systematic review and meta-analysis. Hurting. 2011;152(3):533-42. doi: 10.1016/j.pain.2010.11.002. [PubMed: 21251756].
- 28.
Zeidan F, Martucci KT, Kraft RA, Gordon NS, McHaffie JG, Coghill RC. Brain mechanisms supporting the modulation of pain by mindfulness meditation. J Neurosci. 2011;31(xiv):5540-8. doi: 10.1523/JNEUROSCI.5791-10.2011. [PubMed: 21471390]. [PubMed Primal: PMC3090218].
- 29.
Nascimento P, Costa LOP, Araujo AC, Poitras S, Bilodeau M. Effectiveness of interventions for non-specific depression dorsum pain in older adults. A systematic review and meta-analysis. Physiotherapy. 2019;105(2):147-62. doi: 10.1016/j.physio.2018.11.004. [PubMed: 30563712].
Copyright © 2020, Author(due south). This is an open-access article distributed under the terms of the Artistic Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/) which permits copy and redistribute the material just in noncommercial usages, provided the original work is properly cited.
macandiehaddince1971.blogspot.com
Source: https://brief.land/ijpbs/articles/102509.html
0 Response to "Brief Mindfulness-based Interventions for Acute and Chronic Pain a Systematic Review"
Post a Comment